Download the Doctor Discussion Guide
Seizures may be a sign of something more, so don’t wait to start the conversation with your doctor. This resource will provide you with:
- Important information to share with your doctor that may help lead to a more specific diagnosis
- Conversation starters to help keep your discussion on track
- Useful tips to prepare for your upcoming appointments
- A summary of why each question matters
Download the guide here or view it in its entirety below.
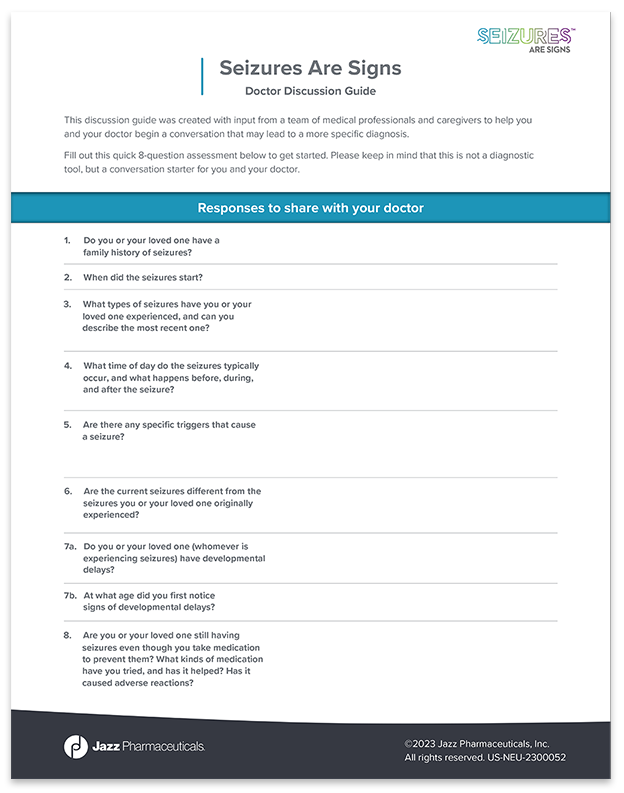
Please keep in mind that this is not a diagnostic tool, but a conversation starter for you and your doctor.
Doctor Discussion Guide
Answer these questions to share with your doctor
- Do you or your loved one have a family history of seizures?
- When did the seizures start?
- What types of seizures have you or your loved one experienced, and can you describe the most recent one?
- What time of day do the seizures typically occur, and what happens before, during, and after the seizure?
- Are there any specific triggers that cause a seizure?
- Are the current seizures different from the seizures you or your loved one originally experienced?
- Do you or your loved one (whomever is experiencing seizures) have developmental delays?
- At what age did you first notice signs of developmental delays?
- Are you or your loved one still having seizures even though you take medication to prevent them? What kinds of medication have you tried, and has it helped? Has it caused adverse reactions?
Questions to start the conversation
These questions were created with input from parents of children and adults living with rare and severe seizure disorders to help you make the most of your appointment. Whether you’re talking to a new doctor or your current doctor, this page was created to help get the conversation started. Keep it for your records.
Before you start, let your doctor know that you read about uncontrolled seizures and wanted to ask a few questions.
- I’m worried about uncontrolled seizures and took an assessment to share with you. Can we talk about the assessment together?
- Is it possible that my loved one has a specific syndrome, and would you recommend doing any additional tests, such as genetic testing?
- Would having a specific diagnosis open up the door to more tailored treatment options or services?
- Is there anyone, in addition to you, who you would recommend we see or make an appointment with?
- How should I be tracking the seizures to help you get the information you need?
- A seizure tracker app
- Virtual hub
- Written log/seizure diary
- Mobile phone videos of the seizures
- Other
- How often should we communicate, and what’s the best way for me to reach you in between appointments or in case of emergency?
4 tips to prepare for your appointment
- Call your doctor’s office and ask the staff if the doctor would prefer that you send questions ahead of time or bring them with you. You can include some of the questions on this page.
- Bring this document along with any relevant medical records, seizure tracker logs, paperwork, and/or video recordings of recent seizures, including what happened before, during, and after.
- Print, save, and review this document ahead of time and jot down any additional notes or questions.
- If you can, bring someone with you to the appointment that can help take notes while you talk to the doctor.
For your records: Why each assessment question matters
The Seizures Are Signs assessment was created with the support of a medical team to help you and your doctor begin a conversation that may lead to a more specific diagnosis. This page is for your background information. Review it before your appointment as a reminder of why each assessment question matters, and keep this page for your records.
- Family history of seizures matters because...
- There are only a few epilepsy syndromes that are hereditary, so this may help your doctor uncover a specific diagnosis sooner, and a simple genetic test may help rule out Lennox-Gastaut syndrome (LGS), Dravet syndrome, or tuberous sclerosis complex (TSC); however, not all seizure disorders are associated with a family history.
- When the seizures started matters because...
- People with LGS tend to experience seizures later in childhood than those with Dravet syndrome or TSC. Unrecognized and/or uncontrolled seizures are linked to developmental delays, learning and behavioral disorders, and other negative long-term outcomes. By catching seizures early on, you and your doctor can develop the right treatment plan.
- Seizure types matter because...
- Every seizure disorder presents with a different combination of seizure types. Seizure types, frequency, and duration are important for a doctor to know and may help uncover an accurate diagnosis.
- The time of day matters because...
- You or your loved one may experience too many seizures to count. However, it’s important to try to take note of the most problematic seizure types, their time of day, and the duration of those seizures, so you can give your doctor a clearer picture of what’s happening. These details could be a clue to a more specific diagnosis.
- Seizure triggers matter because...
- Seizures can be brought on by a number of different triggers. While not everyone experiences triggers, some syndromes, like Dravet syndrome, are triggered by things like heat and illness. If you’re unsure about whether there are triggers, try keeping a seizure diary to help you identify patterns so you can relay them to your doctor.
- Whether or not the current seizures are different matters because...
- Seizures can change and new seizure types may emerge over time. Tracking them helps you identify if they do. This is important information for your doctor to know because some epilepsy syndromes are diagnosed when specific combinations or patterns of seizures emerge.
- Signs of developmental delays matter because...
- This can serve as a potential clue to determining a specific diagnosis. While not everyone will experience developmental delays, early detection can potentially reduce developmental delays or cognitive impairment.
- Still having seizures even though you take medication to prevent them matters because...
- Finding a treatment for uncontrolled seizures can be challenging and the more you know about your specific epilepsy syndrome, the more likely you are to get a treatment regimen that works. Sodium channel blockers, for example, may exacerbate seizures in Dravet syndrome. Knowing what to avoid is just as important as knowing what to take. An accurate diagnosis can help drive to better treatment decisions.